Infección connatal por citomegalovirus
Dr. Juan Gesuele
Asistente de Neonatología
Departamento de Neonatología – CHPR
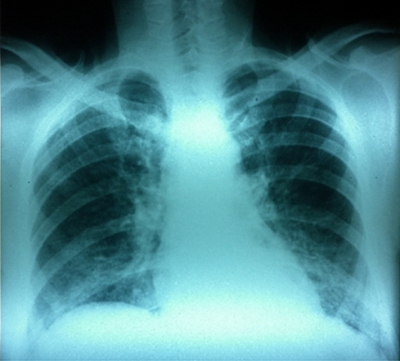
Pneumocistosis en un paciente portador de VIH
Dra. Macarena Vidal
Residente de la Cátedra de Enfermedades Infecciosas
Uso racional de antimicrobianos en el Departamento de Medicina interna de un hospital universitario: resultados de una experiencia piloto
Susana Cabrera A., Leonardo Sosa, Zaida Arteta, Verónica Seija, Soledad Mateos, Abayubá Perna, Mariana Firpo, Gabriela Pereira, Gimena Lombardo, Ximena Añón, Mariela Teliz, Natalia Danese, Maynés López, Jimena Bueno, Cecilia Romero, Raúl Rozada, Virginia Antelo, Ana Laura Quijano y Djalma Oper
Dermatofitosis en paciente VIH positivo
Dra. Beatriz Pi
Postgrado Enfermedades Infecciosas
Facultad de Medicina
Marzo 2012
Normas Nacionales de Diagnóstico, Tratamiento y Prevención de la Tuberculosis en la República Oriental del Uruguay
«En Uruguay, a comienzos de la década de los ochenta del siglo XX, se implantó el Programa Nacional de Control de la Tuberculosis (PNC-TB). Una de las medidas de mayor significación Primeras Normas Nacionales de Tratamiento de la Tuberculosis (TB).
Desde abril de 2006 están en vigencia las actuales NORMAS NACIONALES DE DIAGNÓSTICO, TRATAMIENTO Y PREVENCIÓN DE LA TUBERCULOSIS EN LA REPUBLICA ORIENTAL DEL URUGUAY. Durante el lapso transcurrido la aparición de determinantes socio-económico-culturales que repercuten inexorablemente sobre la epidemiología de la enfermedad, exige una adaptación de esta normativa.»
La Gaceta de Infectología y Microbiología Clínica
Archivos para descarga:
Sanofi Pasteur Travel Grants for Awards for Latin American Women Physician and Scientists
Ceftriaxone and ciprofloxacin restriction in an intensive care unit: less incidence of Acinetobacter spp. and improved susceptibility of Pseudomonas aeruginosa
JULIO CÉSAR MEDINA PRESENTADO, DANIELA PACIEL LÓPEZ, MAXIMILIANO BERRO CASTIGLIONI, AND JORGE GEREZ
Abstract
Objective. To determine whether restricting the use of ceftriaxone and ciprofloxacin could significantly reduce colonization and infection with resistant Gram-negative bacilli (r-GNB). Methods. A two-phase prospective study (before/after design) was conducted in an intensive care unit in two time periods (2004–2006). During phase 1, there was no antibiotic restriction. During phase 2, use of ceftriaxone or ciprofloxacin was restricted. Results. A total of 200 patients were prospectively evaluated. In phase 2, the use of ceftriaxone was reduced by 93.6% (P = 0.0001) and that of ciprofloxacin by 65.1% (P = 0.041), accompanied by a 113.8% increase in use of ampicillin-sulbactam (P = 0.002). During phase 1, 48 GNB were isolated [37 r-GNB (77.1%) and 11 non-r-GNB (22.9%)], compared with a total of 64 during phase 2 [27 r-GNB (42.2%) and 37 non-r-GNB (57.8%)] (P = 0.0002). Acinetobacter spp. was isolated 13 times during phase 1 and 3 times in phase 2 (P = 0.0018). The susceptibility of Pseudomonas aeruginosa to ciprofloxacin increased from 40.0% in phase 1 to 100.0% in phase 2 (P = 0.0108). Conclusions. Restriction of ceftriaxone and ciprofloxacin reduced colonization by Acinetobacter spp. and improved the susceptibility profile of P. aeruginosa.
Publicado en: Rev Panam Salud Publica 30(6), 2011